Author: Dallin Greene, DPM, Glendive Medical Center in Glendive, MT.
Dr. Dallin Greene is a board-certified Foot and Ankle surgeon, treating all aspects of the foot and ankle with
expertise in deformity correction. Dr. Greene graduated from Brigham Young University-Idaho in 2009 with a bachelor’s in biology. He then attended Midwestern University Arizona for a Doctorate in Podiatric Medicine. He completed a three-year surgical residency in foot and ankle trauma and reconstruction in Binghamton, New York. During residency, Dr. Greene received extensive training in foot and ankle arthroscopy and specialized in treating sports injuries, bio-mechanical abnormalities in adults and pediatrics, trauma & wound care. Dr. Greene is board certified with the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine
INTRODUCTION
The posterior tibial tendon (PTT) serves as a primary dynamic stabilizer of the medial longitudinal arch of the foot1. It runs within a groove behind the medial malleolus, strongly attached to the bony surface by the flexor retinaculum2. Posterior tibial tendon dysfunction (PTTD) typically begins with para-tenonitis of the tendon which may lead to synovitis, intrasubstance tearing and tendinosis. More frequent in women and in people older than 50 years of age, further favored by obesity, diabetes, and hypertension, this dysfunction is characterized into four stages2,3. In stage II PTTD the tendon elongates and intrasubstance tears develop, leading to adult acquired flatfoot deformity (AAFD)3. When conservative treatment is unsuccessful, surgical treatment might be necessary. One of the most common surgical approaches for this dysfunction is the Kidner procedure, involving an Accessory Navicular removal and reattachment of the PTT to the undersurface of the navicular body4.
CASE PRESENTATION
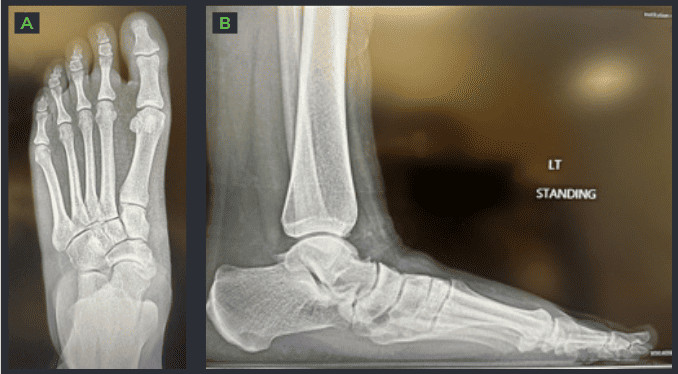
A 23-year-old female patient, weighing 230 pounds. The patient complained of pain along the posterior tibial tendon and medial arch of the left foot for about a year. Pain seemed to improve with decreased activity, yet the patient employment involved standing on her feet all day. After trying conservative treatments, including – custom orthotics, changing shoe gear, physical therapy as well as an ankle brace, the patient experienced some improvement but continued to suffer from pain. Clinical assessment and imaging (MRI & X-Ray) of the left foot supported the following diagnosis:
- Stage II Posterior Tibial Tendon dysfunction
- Left Rearfoot Valgus
- Left Forefoot Varus
- Accessory Navicular
WHY OSSIOfiber® IS AN IDEAL CHOICE FOR THIS PATIENT?
The patient is very young, and the primary goal was to spare her joints and avoid any permanent hardware removal in the future. It was decided that OSSIOfiber® would be the ideal choice of treatment, providing stable fixation and stabilization for the healing period while avoiding the use of permanent hardware.
Preoperative Planning:
A combination of surgical procedures will be performed to manage the patient’s deformity. Medial Slide Calcaneal Osteotomy, Lateral Column Lengthening (Evans Osteotomy), Medial Cuneiform Opening Wedge Osteotomy (Cotton Osteotomy) and Kidner procedure.
Surgical Procedure:
The following fixation implants were used:
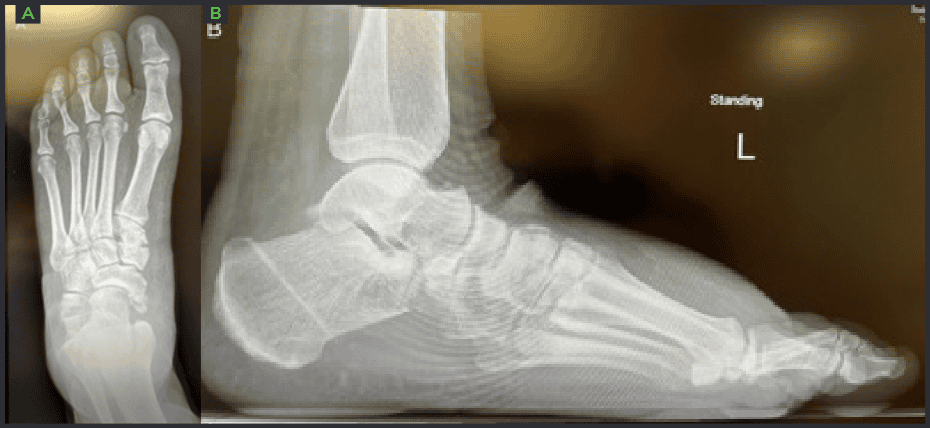
- Calcaneal Slide – A single OSSIOfiber® 4.0x50mm Compression Screw (CS) and 2 OSSIOfiber® 4.0x70mm Cannulated Trimmable Fixation Nails (TFN)
- Evans Osteotomy – Two OSSIOfiber® Compression Staple 15x15mm
- Cotton Osteotomy – A single OSSIOfiber® Compression Staple 15x15mm
- Posterior Tibial Tendon fixation (Kidner procedure) – A single 4.75mm OSSIOfiber® Suture Anchor (SA) White/ Black Tape w/ Needles
Accompanying devices:
- Medline Evans & Cotton 7mm and 8mm Bone Wedges
Surgical Technique Steps:
The patient was placed on the OR table in a supine position. Ipsilateral hip bumped for better lateral exposure.
Calcaneal Slide
- Dissection / Access:
A 5cm incision was made just inferior to the Lateral Malleolus directed posteriorly/ superiorly at a 45° angle, stopping just before the Achilles Tendon. Dissection was carried to bone. - Fixation site preparation:
The periosteum was cut and reflected where the Calcaneal Osteotomy was planned. An osteotomy was then performed using a sagittal saw and stopped just before the medial cortex. The osteotomy was completed using an osteotome and mallet. - Fixation:
The posterior Calcaneus was translocated approximately 1cm medially before placing a 4.0x50mm OSSIOfiber® CS across the osteotomy site, the screw was inserted from the posterior plantar heel. Then, two of the 4.0x70mm OSSIOfiber® TFNs were trimmed to 50 & 55mm and placed across the osteotomy site. - Closure:
Incisions were closed in a layered fashion using 3-0 Vicryl, 4-0 Vicryl and 3-0 Nylon.
Evans Osteotomy
- Dissection / Access:
An incision of about 4cm was made to the lateral side of the foot, it went from the superior anterior process of the Calcaneus in a 45° ankle towards the plantar heel. Dissection was carried to bone. Note – Make sure to retract neurovascular structures and Peroneal Tendons. A cut to the periosteum was made as a guide for an osteotomy, ~1.5cm proximal to the Calcaneal Cuboid joint. - Fixation site preparation:
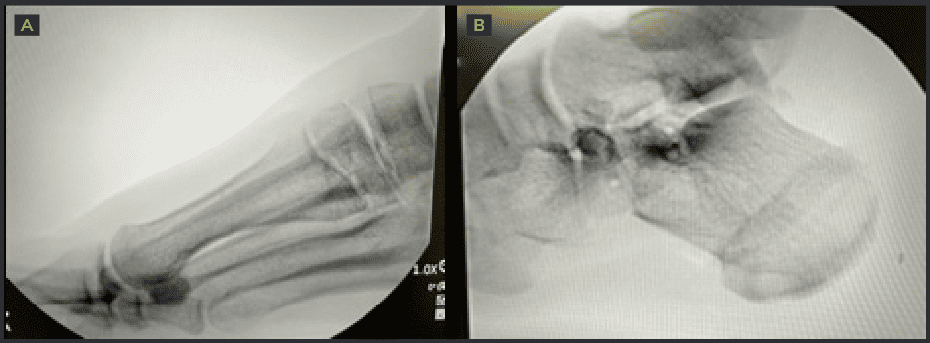
Before doing the osteotomy, a k-wire was placed from just distal to the Calcaneal Cuboid joint into the anterior process of the Calcaneus to prevent dorsal subluxation following the osteotomy. The osteotomy was then performed, a bone distractor was placed over the osteotomy and an 8mm Evan’s bone wedge was planted within the osteotomy. - Fixation:
Two OSSIOfiber® 15x15mm Compression Staples placed over the osteotomy site. - Closure:
The k-wire was removed and layered closure was performed using 3-0 Vicryl, 4-0 Vicryl and 3-0 Nylon. At this point the hip bump was removed.
Kidner Procedure
- Dissection / Access:
A 4cm incision was made over the Navicular Tuberosity. Dissection was carried down to bone and the Posterior Tibial Tendon insertion. - Fixation site preparation:
A portion of the Posterior Tibial Tendon was retracted off its insertion, trying to keep some of the fibers connected if possible. The prominent Navicular is shaved down to remove accessory Navicular. - Fixation:
A single 4.75 OSSIOfiber® Suture Anchor was placed in the Navicular bone. The suture was passed through the Posterior Tibial Tendon, reattaching it to the Navicular bone. - Closure:
Layered closure was performed using 3-0 Vicryl, 4-0 Vicryl and 3-0 Nylon.
Cotton Osteotomy
- Dissection / Access:
A 5cm incision was made over the Medial Cuneiform and dissection was carried down to bone. - Fixation site preparation:
An incision was made through the periosteum at the middle of the Cuneiform followed by an osteotomy through the center of the bone. The osteotomy started while under fluoroscopy to ensure a centered cut in the middle of the Cuneiform. A bone distractor was placed over the osteotomy and a 7mm Cotton bone wedge was planted within the osteotomy. - Fixation:
Once the distractor was removed a single OSSIOfiber® 15x15mm Compression Staple was placed over the osteotomy site. - Closure:
Layered closure was performed using 3-0 Vicryl, 4-0 Vicryl and 3-0 Nylon.
Incisions were dressed with Xeroform gauze, and a dry, sterile dressing followed by a well-padded stir-up splint.
and Calcaneal Osteotomy [B].
Technique Pearls
OSSIOfiber® CS
- Make sure to countersink properly. Using power on insertion of the 4.0 OSSIOfiber® CS is not recommended. It increases risk for stripping the hex.
OSSIOfiber® TFN
- Inserting the OSSIOfiber® cannulated TFNs under fluoroscopy is recommended, to make sure the metal inserter is flush with the bone cortex. This way the implant will not be left proud.
OSSIOfiber® Compression Staple
- Make sure to provide contra-resistance by an assistant on the planter side, when inserting the staples.
Post-Operative Protocol
- Non-weight bearing: For 1 month
- Partial weight bearing: Transition from non-to-full weight bearing over a period of 1 week (progressively
increasing weight each day) - Full weight bearing: At 5 weeks in walking boot
- Comfort shoe: At 10 weeks in supportive stiff tennis shoe
Patient Follow-up
The patient recovered well with pain relief. After non weight bearing for 1 month, she transferred to weight bearing in a walking boot for another month, then with an ankle brace for the 3rd month. The patient is a teacher and worked on her feet long hours, during most of the healing phase. Her foot was in a dependent position more than advised and experienced some swelling, yet still she did well, and swelling resolved. Overall, the patient’s healing process was faster than expected, likely influenced by her young age.
Summary
This is a case of a young teacher with a painful AAFD. While addressing her deformity it was important to spare her joints and avoid metal hardware that could become painful in the future and may lead to removal surgery. The OSSIOfiber® implants provide stable fixation and complement a flatfoot reconstruction very well. While traditionally slightly larger screws are used for Calc Slides, this patient and my other patients have done very well with OSSIOfiber® 4.0 TFNs and Compression Screws.
References
1. Liang, Z. & Lui, T. Endoscopically assisted reconstruction of posterior tibial tendon for stage 2 posterior tibial tendon dysfunction. Arthrosc. Tech. 8, e237–e243 (2019).
2.Zannoni, S., Bonifacini, C., Albano, D., Messina, C. & Sconfienza, L. . Posterior tibial tendon dislocation: a case report. J. Foot
Ankle Surg. 61, 417–420 (2022).
3.Ringleb, S. I. et al. Changes in gait associated with acute stage II posterior tibial tendon dysfunction. Gait Posture 25, 555–564
(2007).
4.Lee, K. T. et al. Midterm outcome of modified Kidner procedure. Foot ankle Int. 33, 122–127 (2012).
Medical professionals must use their professional judgment for patient selection and appropriate technique.
Results from case studies are not predictive of results in other cases. Results may vary.
Please refer to the product instructions for use for warnings, precautions, indications, contraindications and technique.
Some products mentioned in this document may not be currently available or approved for sale in your country. Speak to
your local sales representative/distributor for product availability.
